Since the economy has reopened, most agents have started to see rising footfall, number of transactions, and even commissions earned. However, their business is yet to return to pre-COVID levels. Although CICO agents are the key enablers of social benefits transfers, they have not received any relief or support measures similar to those offered to other enterprises during the pandemic. Our report takes a deeper look at the situation and provides recommendations to the government and financial institutions on initiatives that will boost the transactions and income level of the agents.
NFHS 5 calls for urgent action on child nutrition in India
The percentage of children who are stunted, wasted, underweight, anemic, and obese is on the rise across India. Despite impressive progress in areas, such as water and sanitation—immunization and maternal health indicators of child health alongside nutrition remain a matter of grave concern. UNICEF predicts a further increase in malnutrition by at least 10% in the country, as a result of the COVID-19 crisis.
The Ministry of Health and Family Welfare, Government of India has recently released a report on findings from the first round of the Fifth National Family Health Survey (NFHS 5). The survey covers 17 states and five union territories, which comprise 54% of India’s population, and informs policy on household-level health and nutrition indicators. Since the NFHS is an outcome-level survey, conclusions or attributions on inputs and policies that might have contributed to these outcomes are difficult to draw.
The NFHS has 42 indicators related to child health and nutrition. The trends in neonatal and infant mortality rates from 2015 to 2019 suggest that India has managed to reduce child mortality. Yet the major public health indicators for child health have only improved marginally or not at all, while nutrition-related indicators have worsened in most states. These include stunting (13 out of 22 states and union territories saw an increase), wasting (12 states and union territories saw an increase), underweight (16 states and union territories saw an increase), anemia (16 states and union territories saw an increase), and obesity (all states and union territories except Goa saw an increase).
NFHS-5 child nutrition story
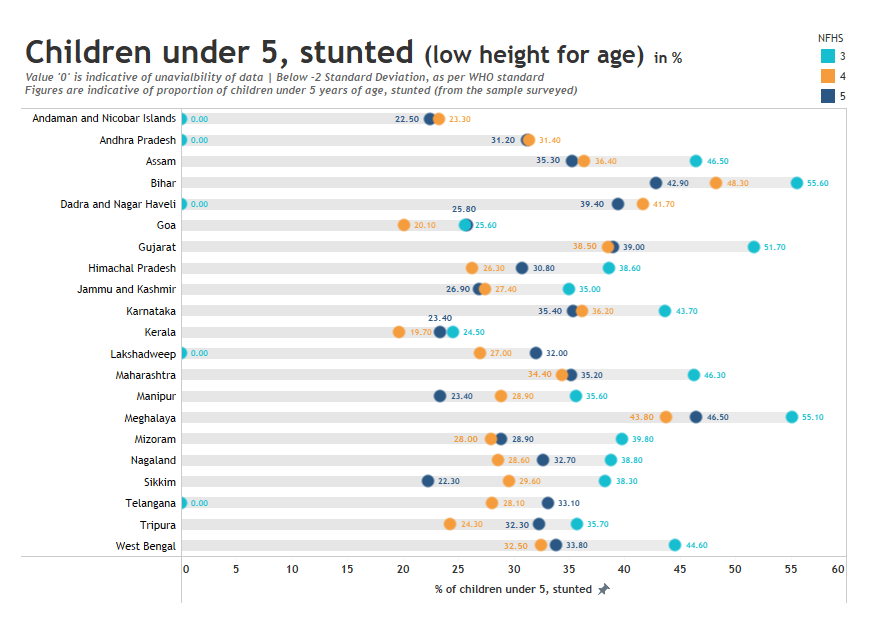
Stunting: The level of stunting, or lower-than-expected height for age, has either deteriorated or improved only marginally in most states and union territories, as compared to NFHS-4 (2015-16). Out of the states surveyed, the levels of stunting worsened in 11 states while others recorded a marginal improvement. The rates of stunting went up significantly in the states of Goa, Kerala, Telangana, and Himachal Pradesh. Tripura emerged as the worst-performing state on the indicator, with a rise from 24.3% to 32.3% in the last four years. Bihar, which had the highest levels of stunting in NFHS-4, saw a marginal decline from 48.3% to 42.9%.
The National Family Health Survey (NFHS) survey is a large-scale nationwide survey of households. The ministry has designated the International Institute of Population Sciences as the nodal agency. Fifth in the series, the factsheet released for states and union territories provides aggregated data on 131 parameters. NFHS-3 was conducted in 2005-06 and NFHS-4 in 2015-16.
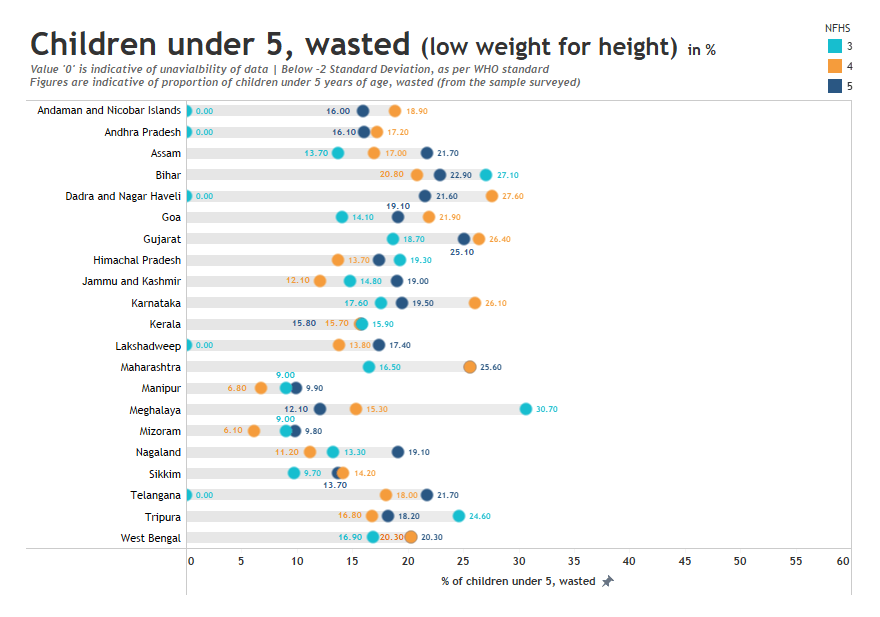
Wasting: The levels of wasting, or lower-than-expected weight for height, saw a similar trend of reversal or stagnation in most states. Of the 21 states and union territories, 10 have reversed on the parameter and the figures are closer to the levels in NFHS-3 (2005-06). Nagaland and the union territories of Jammu and Kashmir increased by six percentage basis points. With a drop from 26.1% to 19.5%, Karnataka emerged as the best-performing state. The states of Meghalaya and Goa also improved as compared to the previous survey.
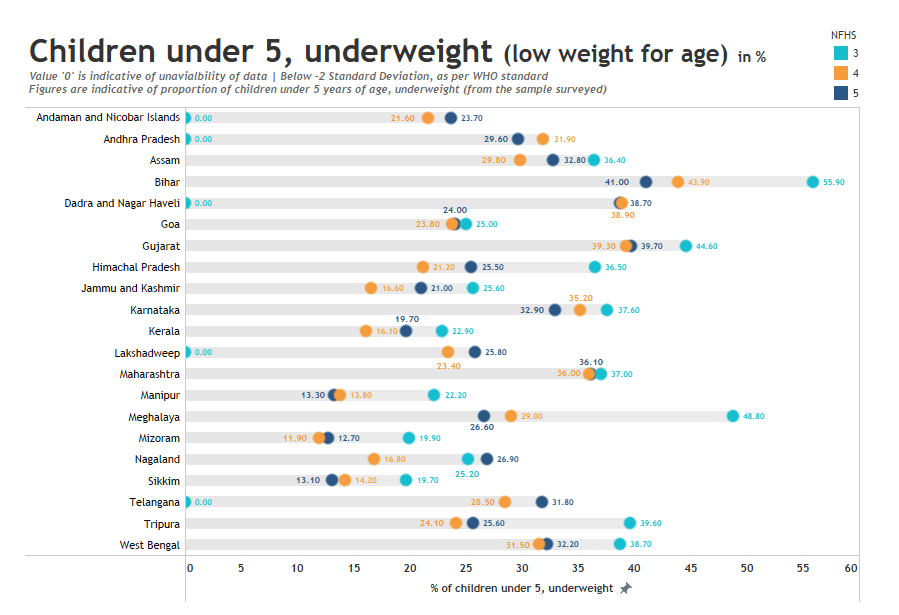
Underweight: Another indicator used to gauge the status of child nutrition is the percentage of underweight children aged five or less. This indicator also showed alarming trends similar to other nutrition parameters. The population of underweight children increased in 11 states and all five union territories. Bihar, Gujarat, and a few northeastern (NE) states saw a marginal to low decline in the levels. However, more affluent states like Kerala and Telangana saw a rise in the proportion of underweight children by almost three percentage basis points. The levels went up from 16.1% to 19.7% in Kerala and from 28.5% to 31.8% in Telangana.
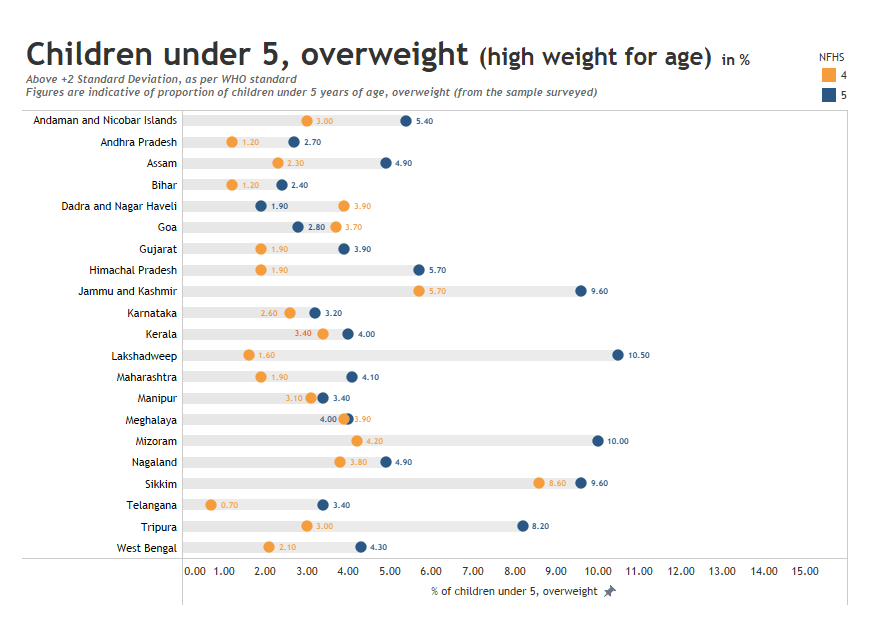
Overweight: Children aged under five are considered overweight if their weight-for-height is two standard deviations above the median of WHO’s Child Growth Standards. Although the proportion in India is within the world average as per WHO, the indicator is under distress. As compared to the previous survey, 16 out of 17 states recorded an increase in the percentage of overweight children in NFHS-5.
With a decrease from 3.7% to 2.8%, Goa was the best-performing state. All other states recorded an increase in the indicator, ranging from 0.1% to 5.8%. The percentage of overweight children more than doubled in Mizoram.
The findings point to a triple burden of malnutrition in India, in terms of stunting, wasting, and child obesity.
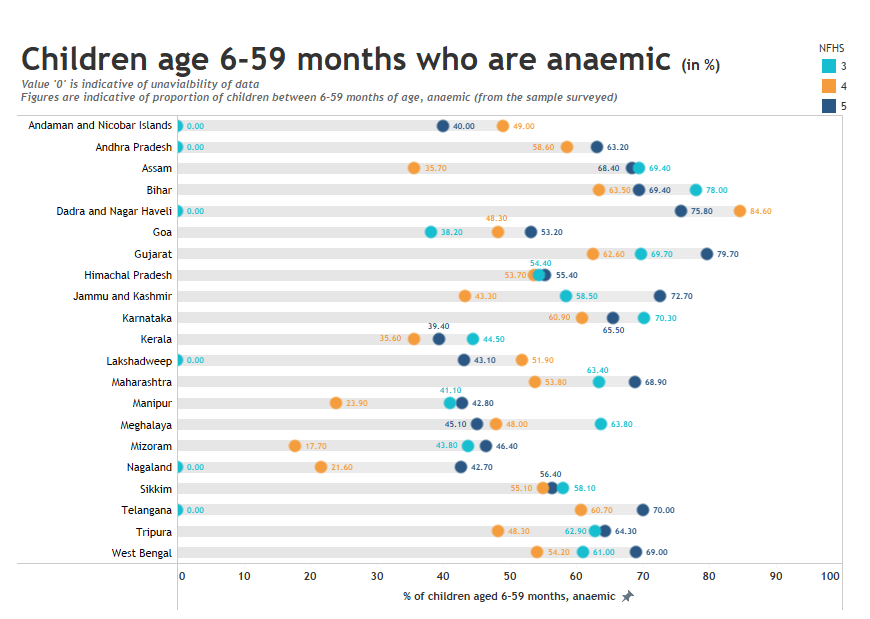
Anemia: The increasing prevalence of anemia among children aged 6-59 months was also worrying. In some states, the prevalence is even higher than that of NFHS-3 (2005-06). For instance, the levels rose from 35.7% to 68.4% in Assam, while Gujarat recorded a 15% increase. Other states also show a major reversal from NFHS 4 levels. The analysis highlights that as compared to NFHS-4, the parameter has worsened in 17 out of the 21 states and union territories, as shown in the graph below.
Though phase 2 data from other states will provide more clarity, these results are certainly a cause for concern and require urgent action. The second phase of NFHS-5 may present even more alarming findings since the survey was carried out after the lockdown-related restrictions were relaxed.
Underutilization of allocated resources
The government must also consider the results of the first phase of NFHS-5 in the context of India’s Mid-Day Meal (MDM) initiative. The Accountability Initiative of the Centre for Policy Research reported that only 14 states utilized 100% of the total funds allocated under MDM in 2018-19, which indicates sub-optimal performance on the ground. Another analysis by the Accountability Initiative shows that only 44% of the government-approved amount for Integrated Child Development Services (ICDS) was utilized in 2018-19. Furthermore, the number of children aged six months to six years who receive benefits under the Supplementary Nutrition Programme (SNP) was less than half the estimated number of beneficiaries in 21 states and union territories between 2017 and 2019.
The economic slowdown and stagnation in wages of the poor have translated to lower consumption, as evident from the expenditure survey of NSSO (2017-18). In this context, the results of NFHS-5 will likely reflect the reduced ability of the poor to access quality nutrition and the inadequate contribution to programs, such as ICDS and MDM, which advance better nutrition.
Need for enhanced focus on nutrition due to COVID-19
The COVID-19 pandemic has the makings of a perfect storm for the existing nutrition crisis. According to the India Child Well-being Report 2020 of World Vision India, more than 115 million children in the country no longer have three meals a day and many continue to miss mid-day meals as schools remain closed. This will have long-term adverse effects on the economic prospects of the country due to reduced schooling and cognitive impairments, and the consequent loss in productivity.
New estimates by Derek Headey and colleagues in The Lancet suggest that without timely action, the global prevalence of child wasting could rise by a shocking 14.3%. In the face of a drastic decline in income, the poor would stop consuming the more expensive nutrient-rich foods to preserve their caloric intake. This would exacerbate the undernutrition crisis. For the poorest and the most vulnerable of India, the effects could be particularly detrimental.
Dalberg’s survey of 47,000 poor households highlights the devastating economic impacts during the lockdown imposed to curb the spread of COVID-19. Primary income earners in two-thirds of surveyed households in the LMI segment lost their jobs or wages during the lockdown, and the average family lost more than 60% of their pre-crisis income. The economic distress, coupled with the halt in the mid-day meal initiative, is expected to lead to a dangerous deterioration in dietary quality.
While the ministry is yet to release granular data for all states and union territories, the consistent reversal on several parameters that gauge child nutrition is apparent from the phase 1 data. The overall trends suggest an improvement in many input indicators, such as access to sanitation, use of cleaner fuels, immunization, maternal health check-ups, exclusive breastfeeding, and adequacy of the diet. Other social determinants of health, including indicators of women’s empowerment, have also improved. However, more focused policy analysis, revised policies, and institutional overhaul are needed to identify and address the multidimensional aspects of child malnutrition.
The drop in performance across child nutrition indicators is a wake-up call for India. The country must take proactive measures and scale-up innovations to address malnutrition. Going forward, the government needs to work on certain quick fixes to address the issue of malnutrition. These could include:
- Dietary diversification at the household level, as part of the national nutrition strategy for effective supplementation of micronutrients;
- Launch and scale-up of innovations with a focus on improvement in healthcare and nutrition among children. These would include the promotion of exclusive breastfeeding, food fortification across PDS, ICDS, and MDM, enhanced care, referrals and management of severely undernourished and sick children, effective implementation of Vitamin A supplements to children up to the age of five, and regular deworming;
- Enhanced emphasis on nutrition literacy at the household level;
- Adoption of alternate delivery channels like cash transfer pilots in high-burden districts to encourage dietary diversification.
References;
[1] The National Family Health Survey (NFHS) survey is a large-scale nationwide survey of households. The ministry has designated the International Institute of Population Sciences as the nodal agency. Fifth in the series, the factsheet released for states and union territories provides aggregated data on 131 parameters. NFHS-3 was conducted in 2005-06 and NFHS-4 in 2015-16.
Reimagining the Indian government’s telemedicine platform
1. Background
Toward the end of December, 2020, The Times of India reported incidents of sexual harassment on Indian telemedicine platforms that offer consultations with doctors. The report noted that these platforms “have become sites for sexual harassment of women doctors, with ‘patients’ flashing, masturbating or making lewd conversation in the guise of seeking consultation.” The report went on to state that instead of informing the police of such incidents, the platforms kept it under wraps and implemented additional measures to prevent such incidents, without much success. While the report mentions the misuse of some private platforms, it does not mention whether eSanjeevani, the telemedicine platform of the Government of India where more than 1 million consultations have been recorded until the end of December, faced similar issues.
eSanjeevani had its genesis on 25th March, 2020 when the Medical Council of India (MCI) and NITI Aayog jointly released the telemedicine practice guidelines. These guidelines enable Registered Medical Practitioners (RMPs) to provide healthcare remotely using digital platforms. Soon after, on 13th April, 2020, the Ministry of Health and Family Welfare (MoHFW) launched eSanjeevani, a platform that offers remote health services. Private sector players, such as Practo, 1mg, among others, also rapidly launched their telemedicine services.
Telemedicine is not new to India. As early as 2009, Health Point Services (HPS) launched a telemedicine offering, eHealthpoint (eHP), in Punjab. However, eHP did not gain much traction. A decade later, the delivery of health services online is now an attractive proposition. This was possible through India’s robust telecommunication infrastructure and ubiquitous availability of the 4G network. The low cost of data, a result of competition among telecom players, as well as high mobile penetration also played a major role in this transition. The COVID-19 pandemic further accelerated the need for remote healthcare and consultation.
2. The government’s telemedicine platform: e-Sanjeevani
eSanjeevani seeks to improve access to health services that had been severely curtailed during the pandemic. This was due to movement restrictions imposed during the lockdown and due to the lack of available health infrastructure as a result of COVID-19. The Centre for Development of Advanced Computing (CDAC) developed and launched eSanjeevani in record time. The platform is available in the following two variations:
- Doctor-to-doctor teleconsultations, provided through eSanjeevani Ayushman Bharat–Health and Wellness Centres (AB-HWC): This is deployed in 6,000 HWCs and is served by specialists and doctors in around 240 hubs. More than 20,000 paramedics, doctors, and specialists received training to use eSanjeevani AB-HWC.
- Doctor-to-patient teleconsultations, provided free of cost through the eSanjeevaniOPD platform: eSanjeevaniOPD enables contactless consultations between a doctor and a patient. Approximately 8,000 doctors received training and were onboarded on eSanjeevaniOPD.
As per the Press Information Bureau on 14th December, 2020, the 1 million consultations recorded until December included more than 200,000 doctor-to-doctor consultations and more than 750,000 doctor-to-patient consultations.
3. Addressing the three “As” in eSanjeevaniOPD: Abuse, availability, and access
While it is commendable that the government reacted with alacrity and agility to ensure health services were available in remote areas, the eSanjeevani platform faces three main issues, which are discussed below.
Abuse: The verification process involved in the registration is similar to that of private platforms, which makes eSanjeevaniOPD susceptible to abuse. A patient must register on the platform before they can use it. The two-step process requires a patient to first verify their mobile number through a one-time password (OTP). Subsequently, they must complete a registration form that includes personally identifiable information (PII), such as name, age, biological sex, and address. To simplify the registration process, no proof of identity is requested at the time of registration. This makes it easy for potential abusers to misrepresent their details and enter the platform without being traced back. The OTP verification only serves to confirm whether the patient can access the mobile number provided during registration. It does not provide additional verification features that can enable law enforcement agencies to trace back the number in case of misuse.
One way to address the issue of abuse mentioned in the article of The Times of India is to use Aadhaar verification during the registration process where an OTP would be sent to the mobile number registered against the person’s Aadhaar. However, this would complicate the registration process and as many do not have their Aadhar linked with their mobile numbers, they would not be able to use the platform. Another way to address abuse in the platform would be to match doctors and patients algorithmically, based on biological sex. This will discourage those who sign up to misuse the platform. Users of the eSanjeevani platform confirmed that male patients were matched with female doctors. This could potentially lead to misuse, similar to incidents reported on private platforms. Moreover, as mentioned explicitly in the telemedicine guidelines, consultations should not be anonymous and both the patient and the doctor need to know each other’s identity. This enables the platform to identify any misrepresentations and take necessary action.
Availability: Doctors, particularly women, who have faced such abuse on these platforms may decline to provide online consultations going forward. This would further reduce the availability of healthcare professionals necessary for the platform to function effectively. eSanjeevani already struggles with a shortage of doctors, which is evident by the time it takes for a patient to receive relevant advice after they request a consultation. Patients recounted incidents where doctors were not readily available, which resulted in long waiting times. They mentioned that it sometimes took more than an hour to consult a doctor, with no indication of the time it would take for a doctor to become available.
Although the portal provides patients with an option to select specialist consultation services through a drop-down menu during registration, patients often receive a message stating that the selected service is closed. Patients then try to avail of a general service where the doctor may not be qualified to diagnose the problem, which can lead to an unsuccessful consultation. This suboptimal experience could discourage them from trying to use the platform again. Besides onboarding more doctors, the platform can provide an option for patients to record their symptoms or ailments when they first seek a consultation. The patient can either type it in their chosen language or record an audio message. Using natural language processing (NLP), the platform can then initiate an algorithmic match between a doctor and a patient to reduce unsuccessful consultations.
Access: While telemedicine practice guidelines allow for video, audio, text-based, and asynchronous modes of communication for teleconsultation, the eSanjeevani platform is solely video-based. This requires the patient to have a smartphone or a laptop with an internet connection. The eSanjeevaniOPD application makes remote health consultation accessible to those with such technology. However, it does not solve the problem for digitally excluded individuals and communities, which include those with feature phones that have no internet connectivity or those who do not own a mobile phone. As of October, 2019, approximately half of India’s population was digitally excluded. Even among those who own a mobile phone, 40% remain digitally excluded. Moreover, the patient must also complete the registration forms before they can initiate a teleconsultation and navigate through the appointment process. This requires a knowledge of the English language since the forms and instructions are only available in English. To ensure that such services are accessible to all, governments should set up functional teleconsultation helplines, auto-diallers, text messages, and other asynchronous channels as these modes are permissible under the telemedicine guidelines.
The government can also use community-based digital centers equipped with mobiles or tablets to increase access, such as panchayat (village level government) offices and Self-Help Groups (SHGs). Governments that do not make adequate investments in these channels risk excluding their “digitally limited” segments of the population, thereby depriving them of access to healthcare. This could lead to a situation where the most vulnerable populations with limited access to healthcare cannot access remote healthcare services as well.
4. The way forward: Benchmarking eSanjeevani to global platforms
Besides strengthening eSanjeevani along the lines of the three As discussed above, it can also benefit from offering a wider variety of services similar to other online health platforms based in India and overseas. To reimagine more diversified service offerings on the eSanjeevaniOPD platform, we benchmarked services offered in the teleconsultation space by eSanjeevani, Practo and 1mg in India, Ping An Good Doctor (PAGD) in China, and Amwell and Teladoc in the USA. Some of the services available on these platforms include online consultations, e-health profiles, express drug delivery, health management plans, appointment services, health check-ups, hospital referrals, second opinions, inpatient arrangements, and domestic or overseas medical services (see Appendix-2 for description of the services). The table below highlights the services these platforms provide.

As evident from the benchmarking analysis provided above, there is an untapped opportunity to build eSanjeevani into a world-class teleconsultation platform. This is possible by integrating it within the larger healthcare ecosystem that connects hospitals, clinics, pharmacies, laboratories, diagnostic centers, and doctors who offer in-person consultations. This could be pursued through the National Digital health Mission (NDHM) of the Government of India. However, the government must first address the three “As” of abuse, availability, and access.
Appendix 1: Various health platforms used for comparative study
Practo is a platform based in India that seeks to simplify healthcare by connecting the entire healthcare ecosystem, which includes patients, doctors, pharmacies, diagnostics, clinics, hospitals, and testing labs, among others. Patients can consult doctors virtually and book appointments with them for in-person consultations, order medicines, as well as book tests and check-ups. Practo offers a management software to clinics and hospitals to facilitate activities, such as appointment booking. It enables doctors to create their profiles to increase their online presence and offer online consultations and also allows patients to make appointments for offline consultations. 1mg is another Indian online healthcare service that serves primarily as an online pharmacy. It also offers online consultations and allows patients to book lab tests.
1mg is an online health platform operating in India. 1mg aims to make access to healthcare a hassle-free experience by addressing all health needs of an individual remotely. One can avail of allopathic, ayurvedic, homeopathic medicines, vitamins & nutrition supplements and other health-related products delivered at home. The company also collects samples for lab tests at the patient’s home and provides a platform to consult doctors.
Ping An Good Doctor (PAGD) is a healthcare software company that operates in China, headquartered in Shanghai. PAGD utilizes the internet and artificial intelligence (AI) to address gaps in the Chinese healthcare system. Its objective is to become a one-stop healthcare platform by integrating healthcare information, medical services, drugs, health supplements and equipment, as well as health plans. This includes doctors, hospitals, pharmacies, physiotherapy centers, health check-ups, fitness, beauty care, insurance, and e-commerce. PAGD offers online consultations, e-health profiles, express drug delivery, health management plans, health headlines, centralized appointment services for offline consultation, health check-ups, hospital referrals, second opinion, inpatient arrangements, and domestic or overseas medical services (medical tourism).
Amwell is a telemedicine company based in Boston, Massachusetts that connects patients with doctors over video calls. For healthcare providers, Amwell sells its platform as a subscription service to place their medical professionals online. Its software development kits, APIs, and system integrations enable clients to embed their system into existing workflows.
Teladoc Health, Inc. is a telemedicine and virtual healthcare company based in the US. It provides telehealth services, medical opinions, AI and analytics, and licensable platform services. Teladoc Health uses telephone, video conferencing, and mobile apps to provide on-demand remote medical care.
Appendix 2: Description of the services that have been used for benchmarking telemedicine platforms
Online consultation: Patients can talk to physicians online and consult them through video or voice calls for diagnosis, prescriptions, and other services
E-health profile: Digital version of a patient’s health chart that includes real-time health records, which capture their medical history, diagnoses, medications, treatment plans, immunization records, test results, etc.
Express drug delivery: Medicines can be delivered to patients soon after a consultation, through a delivery platform
Health plans: Customized health plans based on e-health profiles of patients
Appointment services: Booking of appointments through a centralized system
Health check-up: Thorough physical examination, including a variety of tests based on the age and health of a person
Hospital referral: After consultation with a physician, if more advanced care is required, the doctor can refer the patient to a hospital
Second opinion: After an unsatisfactory diagnosis, a patient can request to consult a different doctor for a second opinion
Inpatient arrangement: Arrangement for admitting patients to a hospital for surgery or other procedures
Domestic/ overseas services: Travel arrangement for patients who wish to travel to a different location for medical treatment or care
Designing new-age Government to Citizens (G2C) applications based on the principles of “Technology as a public good’’ and a microservices based architecture
As India grappled with the COVID-19 pandemic, state governments launched various mobile and web applications to deliver social welfare and essential services and disseminate reliable information, among others. These applications differ significantly from each other in terms of their features, development approach, and data privacy. This policy brief proposes a paradigm shift to a more interoperable, open, APIs-based federated microservices architecture. The central and state governments can use this architecture to co-develop government-to-citizen (G2C) applications while ensuring adequate data privacy and standardization.
Digital ID in the time of COVID-19 in India
India’s social welfare delivery system relies on Aadhaar, a biometric digital ID system, to identify and authenticate beneficiaries. About 800 million people use biometric authentication to receive highly subsidized rations every month through the Public Distribution System (PDS). Similarly, millions of beneficiaries use biometric authentication to withdraw money that they receive from social welfare programs and other sources through bank agents, known as business correspondents (BCs). Almost all these transactions rely on a single technology, that is, fingerprint-based authentication.
On 25th March, 2020, the Government of India (GoI) announced an unprecedented nationwide lockdown to curtail the spread of COVID-19. To mitigate the lockdown’s social and economic impact, the GoI rolled out several measures related to welfare and relief. The Pradhan Mantri Garib Kalyan Yojana (PMGKY) was the first such measure and included free food grains and cash aid for the poor and vulnerable segments.
During the lockdown period, and even now, fingerprint-based technology was the primary mode for beneficiaries to authenticate themselves to access benefits under the PMGKY and other social benefit transfer programs. The high-contact nature of fingerprint technology created apprehension among service delivery agents and beneficiaries due to the risk of COVID-19 transmission. In the absence of any reliable alternate technology, they had no other option but to use their fingerprint.
Alternative modes of authentication have been required for a long time, primarily to reduce failure and manage exceptions. For example, studies show that out of the ~7 million Aadhaar-enabled payment system (AePS) transactions between December 2014-2018 facilitated by Business Correspondents (BCs), 34% failed – of which 17% were due to biometric mismatch. During April, 2020, while the lockdown was in effect and vulnerable populations tried to access their cash benefits, cash withdrawal transactions through the Aadhaar-enabled payment system (AePS) were as high as 403 million, which was almost double the transactions in the previous months.
In line with this increase, the rate at which transactions failed in AePS was 39%. The main reason for such failures was a mismatch in biometric data. With limited to no exception handling procedures in place, this high rate of failure translated to millions of distressed and disadvantaged citizens who failed to withdraw cash. Instances of fingerprint authentication failure in the PDS, the most extensive government program to use Aadhaar, have also been reported for a long time.
In this context, this blog examines the constraints that arise from the deployment of just one contact-based biometric authentication technology to avail government benefits. It also identifies contactless technologies to mitigate some of the challenges associated with fingerprint authentication.
The adoption of contactless biometric technology
Iris and facial recognition are two viable alternatives to fingerprint authentication that offer the highest level of security, that is, validation of who you are, which characterizes India’s biometric authentication process. The table below benchmarks, these authentication technologies across various observable parameters:
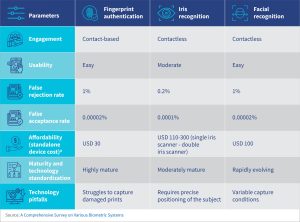
Fingerprint matching technology is accurate and has proven to be highly scalable. However, it struggles to read damaged prints and requires users to physically place their fingers on a surface, a risky proposition during a global pandemic.
Iris recognition has the advantage of high-speed authentication, is highly accurate and mature, and relies on scanning the iris, which is less prone to degradation over time than one’s fingerprints, as with the case of the elderly or those engaged in heavy manual labor. However, successful usage depends on user training as the devices require specific positioning of the iris. Success also depends on robust internet connectivity, as the data packet transmitted to the Aadhaar central repository for authentication is much larger than that of the fingerprint-based system.
Another feasible contactless technology is facial recognition technology (FRT), which relies on consistent facial features despite aging or surgery or both. This biometric technology is affordable and widely available as part of multifunctional devices and across form factors, making it cost-effective and potentially scalable. Globally, law enforcement agencies dominate the use-cases for FRT. Yet more recently, India has utilized FRT for digital ID authentication.
In the past, the country was conservative in its adoption of FRT for ID authentication owing to concerns around privacy and existing investments in fingerprint and iris scanners. However, the tide seems to be turning, in part due to studies that have shown the effectiveness of facial identification. In August 2018, the Unique Identification Authority of India (UIDAI) formally included FRT as an option for Aadhaar authentication. Sector experts have been deliberating about the potential to identify and track COVID-19-positive Indian citizens using Aadhaar-integrated cameras equipped with thermal scanners. UIDAI currently holds images and contact details for approximately 1.23 billion people which can be leveraged after assessing the quality of images captured.
FRT case study: Bangladesh
In October 2019, Bangladesh conducted its first Electronic Know Your Customer (eKYC) pilot. Rather than relying solely on the current practice of four-finger biometric authentication, the government opted to try its home-grown FRT created by Giga Tech Ltd. Of the total 19 banks participating in the pilot, approximately half were assigned fingerprint authentication technology, while the remainder received FRT. Bank employees and agents confirmed the relative ease of using camera phones or tablets to capture beneficiaries’ photos and complete the e-KYC process. Although fingerprint authentication was more readily adopted due to familiarity with the technology, FRT was found to be an efficient contactless technology on par with fingerprint technology. Despite the pilot’s short-term nature, MSC’s analysis suggests that standardizing the biometric devices in terms of hardware and software specifications, issuing detailed FRT instructions, and delivering training sessions would make FRT a leading contender in e-KYC systems.
Let us consider equipping the PDS with alternate technologies—iris or FRT—in addition to the existing fingerprint-based ePoS. Equipping all the fair price shops (FPS) in India with an iris scanner that can be integrated with the existing ePoS will cost USD 60-163 million. For FRT, this cost will be around USD 54 million if a phone or device is also provided to all FPSs. However, the cost would be negligible if the dealers already possess a smartphone and only an agnostic software application needs to be developed.
Adopting other exception management protocols
Besides adopting a nascent technology such as FRT, it is also possible to work within the confines of existing authentication infrastructure to ensure the safety of India’s citizens while limiting exclusions. Such approaches entail the active use of exception management protocols, such as one-time passwords (OTP). This is already part of the protocol for PDS. During the lockdown, PDS dealers in Rajasthan and Karnataka conducted exception handling through OTPs.
As per the Indian Telecom Services Performance Indicator Report as of June 2020, India’s average teledensity was 85.85%, with urban and rural teledensity at 137.35% and 58.96%, respectively. Such widespread mobile penetration makes OTP-based ID authentication feasible, safe, and cost-effective. Moreover, citizens with an Aadhaar card are encouraged to register their mobile numbers to avail different services. Therefore, mobile numbers are already linked to Aadhaar cards, and no additional effort or data collection is required to use this exception management mechanism.
Requesting and using an OTP ensures a satisfactory level of contactless identity authentication and reduces exclusions due to worn fingerprints or interrupted service, resulting in a smooth flow of benefits. However, the challenge in this method is that the most vulnerable populations still might not have access to a phone or may change their numbers frequently.
Conclusion
The COVID-19 pandemic has seen the beneficiaries of the government’s welfare programs either being increasingly excluded or inconvenienced due to the reliance on a single mode of authentication. Biometric-based ID solutions were rolled out, in part, to address such exclusions. However, the contact-based nature of fingerprint technology potentially creates additional health risks for millions of vulnerable people.
The solution may not lie in phasing out or eliminating fingerprint authentication but in providing safer, contactless, and alternative verification options using different technologies. This would ultimately avoid exclusions and ideally eliminate them. Currently, exception handling technologies are sparse, and their usage sporadic. For example, in PDS delivery, only eight states have reported Aadhaar authentication using iris scanners. In the case of banking services, alternate technologies are limited to small-scale pilots.
The newer technologies we covered in this blog have the potential to coexist as robust alternative methods of identity verification to not only assure beneficiary safety but ensure the delivery of benefits. Deploying alternative technologies should be done after considering factors like areas with higher rates of failure, network and server issues, and last-mile service providers’ ability to afford and operate the devices. The government can adopt a phased approach to test the technology after running pilots to ensure that the transition is smooth and sustainable. It has become critical to strike a balance between identifying the recipient accurately, preventing pilferage and delivering government benefits without interruptions. Innovation in the area of authentication technology will be a meaningful step toward achieving this symbiosis.
Public Distribution System spending by the Indian government





