Climate change: A test for resilience of mental health systems?
by Puneet Khanduja and Anirooddha Mukherjee
Apr 29, 2024
5 min
Climate change has a significant impact on human health, particularly on vulnerable groups. Extreme weather events, infectious diseases, and food system disruptions contribute to health shocks, including mental health issues. To address these concerns, India must invest in mental health infrastructure, collaborate with government agencies, civil society organizations, and local communities, and integrate mental health considerations into climate change adaptation and disaster response policies.
Introduction
Well before the COVID-19 pandemic disrupted global health systems and moved the needle for adopting a focused approach to the intersectionality of climate change and health, climate change had been proclaimed as a medical and health emergency by leading organizations devoted to public health, environmental health, patient advocacy, medical practice, and nursing services.
Many global and regional discussions and studies have highlighted the harmful impact of climate change on human health, prompting a One Health approach to health systems. However, these discussions often focus on the physical effects on people and animals, overlooking climate change’s lesser-known mental and psychosocial impacts, particularly on vulnerable groups.
Climate change and human health
Climate change has diverse impacts on the overall health of the affected population, leading to increased risks of mortality and illness from extreme weather events like heat waves, storms, and floods. As our planet warms due to climate change, infectious diseases, particularly zoonotic diseases, i.e., diseases that are transmitted from animals to humans (Ex. COVID-19, Rabies, Anthrax, etc.), are expanding their geographic range beyond traditional warmer latitudes. Extreme climate events also disrupt food systems and worsen issues related to food and water, thus contributing to health shocks, including mental health concerns.
There is clear evidence demonstrating the impact of climate change on mental health. Extreme weather events significantly aggravate stress and anxiety. They may lead to severe clinical conditions like depression, post-traumatic stress disorder (PTSD), and, in many cases, substance abuse disorders.
Children and older adults are more vulnerable to the mental health impacts of climate change. In children, factors such as physiological development, cognitive abilities, and emotional skills intersect with other threats like parental health, depression, anxiety, and poverty. In comparison, older adults face greater physiological susceptibility to climate-related health effects, compounded by factors like physical disabilities and limited access to resources and care.
Furthermore, climate change undermines factors crucial for good health, such as stable livelihoods, societal equality, and access to healthcare and support networks, disproportionately affecting marginalized and vulnerable groups like women, children, ethnic minorities, impoverished communities, migrants, older individuals, and those with pre-existing health conditions.
Dual burden of climate change
Extreme climatic events also impose a significant financial burden on vulnerable communities. These communities, already grappling with limited resources and socioeconomic challenges, bear the brunt of the economic fallout from climate-related disasters. The United Nations highlights how climate change accelerates financial burdens, particularly affecting those most vulnerable and impoverished. For instance, when extreme weather events strike, such as hurricanes, floods, or wildfires, these vulnerable groups often lack adequate insurance coverage or financial reserves to cope with the damages to their homes, businesses, and livelihoods. Global economies such as the European Union have experienced extreme weather and climate events that pose risks to debt sustainability. Financial resilience to climate change is still an under-explored and underfunded theme in India.
Extreme weather events also lead to supply chain disruptions such as transportation issues, labor troubles, and raw materials shortages. The cost of rebuilding and recovery further exacerbates the financial instability of vulnerable communities, perpetuating a cycle of poverty and stress.
Mental health burden in India
India faces a significant mental health burden, with a large portion of the population in need of care but lacking access to services. The utilization of mental health solutions is low, with only 30 percent of mental health patients receiving help and a significant treatment gap across various psychiatric disorders. The mental health infrastructure is inadequate, with a scarcity of mental health professionals and limited resources, especially in rural areas. The overall availability of qualified mental health personnel in the public and private sector is scarce, with only 898 clinical psychologists and 1,500 psychiatric nurses compared to a demand of 3,000, as reported to the Lok Sabha in 2018. The cost of accessing mental healthcare in India is high, with private therapy costing anywhere between INR 1,500 to 3000 (USD ~20 to 40) per session. Access to care is limited, particularly in rural areas, which struggle with a deeper stigma associated with mental health. The stigma associated with mental health in India is a significant issue that affects the quality of mental health care and contributes to the hidden burden of mental health disorders. This stigma takes various forms, including public and self-stigma, and can be influenced by cultural, social, and economic factors and is driven by a pronounced lack of societal support and self-awareness.
Building a climate-resilient healthcare ecosystem in India
The Government of India has made several policies and programmatic steps to address these concerns, such as the Mental Healthcare Act 2017 of 2017 and the District Mental Health Programme (DMHP), built on the Bellary model, to detect, manage, and treat mental health concerns.
However, strategic investments in mental health infrastructure, including expanding services and training healthcare professionals, are crucial. Collaboration between government agencies, civil society organizations, and local communities is essential to develop holistic and culturally sensitive approaches to mental health resilience.
Further, a comprehensive community-driven, locally-led adaptation of the directives in the Mental Health Act, 2017, spearheaded by the State Governments and district administrations, will initiate a much-needed feedback mechanism for impact. Utilizing technology-enabled mental healthcare platforms can be a vital link between youth and community action.
Lastly, integrating mental health considerations into climate change adaptation and disaster response policies is vital to prioritize mental health needs during crises. More profound research on climate-resilient mental health systems is critical to inform evidence-based policies and interventions. Understanding the vulnerabilities of different population groups and identifying best practices for building community-based resilience at various levels is key to addressing the mental health challenges posed by climate change.
India must urgently address the intersection of climate change and mental health to ensure the well-being of its population, especially the most vulnerable. By integrating mental health resilience into climate change policies, India can take significant strides towards safeguarding mental health in the face of climate challenges. It is time for concerted efforts and collaborative actions to build a more resilient health system to effectively mitigate the mental health impacts of climate change in India.
Written by

Puneet Khanduja
Senior Manager
 by
by  Apr 29, 2024
Apr 29, 2024 5 min
5 min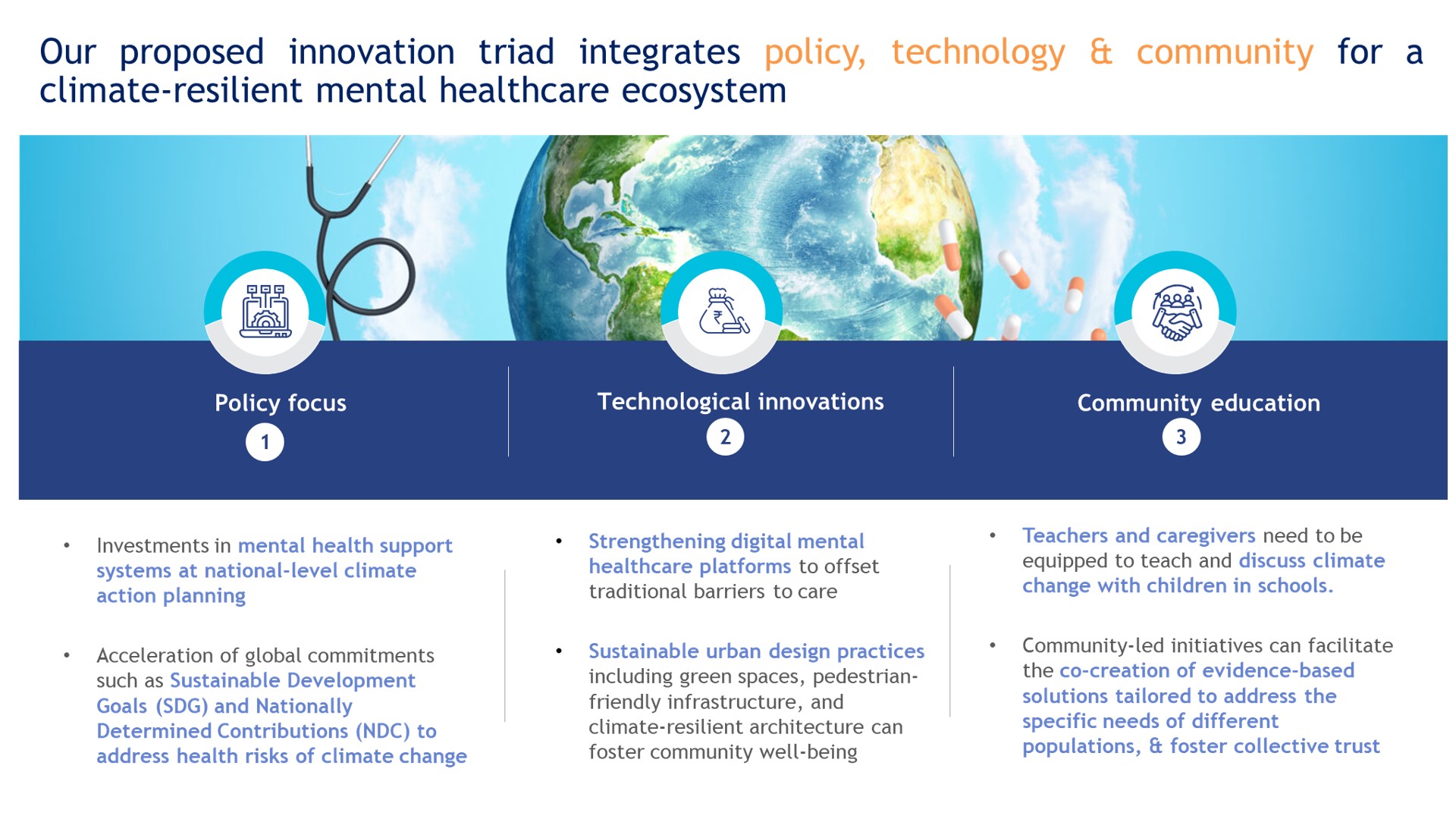
Leave comments